A 45 year old female, agricultural labourer by profession
who was apparently alright until July of 2018 when she developed symptoms of
giddiness, headache, vomiting and generalised weakness. She went to a local
rural medical practitioner (RMP) who did her random blood glucose test using a
glucometer which showed "hi" (usually glucometer in India, show
"hi" when blood glucose level is more than 600mg/dl) Before that she
never got her blood glucose levels checked. The RMP referred to the GP where
she was given oral hypoglycemic drugs among other drugs for symptomatic
management and was sent home.
She was apparently normal for a month when she again developed symptoms of vomiting
and generalised weakness for which they have consulted the RMP who have
referred them to the expert where she was diagnosed as Hyperosmolar
Hyperglycaemic State (HHS) and was administered Inj. Insulin Mixtard (an
intermediate acting insulin) and sent home after her sugar levels normalised.
She was asked to take 10 units of Insulin Mixtard in the morning and 12 units
in the evening.
On 13th May 2019, there was a stressful event in her home, and she happened to
miss her dose of insulin followed by next day morning too. On 14th May 2019
around 11 o clock she developed symptoms of breathlessness, nausea, headache,
burning micturition, abdominal discomfort, and generalised weakness. For which
she was admitted in a local hospital upon consulting the RMP where she was
given I.V. glucose and immediately refereed to our tertiary care hospital where
the random blood sugar level came out to be 440 mg/dl
She was stabilized and up on further investigating from the treating team it has
been found that she was taking Inj. Insulin Actrapid instead of the Insulin
Mixtard which was the recommendation.
Based on the history that the inj which she was taking was a clear fluid where as
actrapid is clear while mixtard is milky.
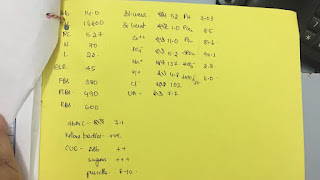
Owing to her history and judging by her presenting complaints, other tests were done
on which the significant findings were of pH which was 7.05, pCO2 was 6.5
and urine ketone bodies were present.
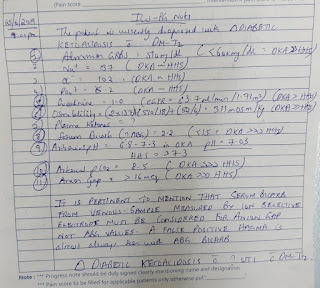
Judging by all these factors she was diagnosed as Diabetic Keto Acidosis (DKA) and her
treatment was started giving insulin infusion.
Her blood sugars levels, ketone body presence and arterial blood gases were
monitored until she could be normalised.
The patients requested an early discharge because they were not able to afford the
stay in the hospital because of the out of pocket expenditure for the patients (for
both medications and stay in the hospital).
The patients and the next to kin are unaware of her parents history of diabetes but
her siblings (Brother and sister) were also diagnosed with diabetes.
CDSS of Readmission of the patient:
12:29 - MS: The patient glucose value has given to more than 600 when she
reached the hospital. She was given IV administration and tablets were
given.
Today
morning when she told tablets she had vomitings, shortness of breath and
dizziness.
They are
thinking to come to hospital now sir.
12:37 - SG: Do we know the reason for her
Hyperglycaemic episode? Did she miss her dose?
12:38 - MS: No bro. As what he has told me she was taking her doses regularly.
I also asked are they correct medications and he said yes.
12:38 - MS: I think we need to check that
12:48 - VP: Any signs of infection?
12:49 - MS: I haven't asked him.
13:38 - RB: Do we have an image of her past
discharge summary from previous hospital?
14:51 - MS: The patient relative informs she is
admitted in hospital
16:18 - RB: Yes we have admitted her.
Will keep you posted
20:35 -: have seen the case .c/o giddiness since
yesterday, breathlessness since morning,2 episodes of vomiting s in the
morning..
20:35 - : what to be started for her sugars??
20:35 - : present grbs 510,pr 110, bp 150/100,RR 35
20:35 - : We discussed that she needs to be begun
on iv insulin DKA algorithm
20:35 - : ohk
20:35 - : What's her blood sugar in first
hour of insulin? How much fluids has she received?
20:35 - : 1lit of bolus followed by 100ml/hr
20:35 - : sir here its given ..once it is less than
250 ,add dextrose ..so should we???
20:35
- : now the grbs is 218
20:35 - : The fact that her Hba1c
looks normal in the face of normal Hb means that she was well controlled at
home and the current crisis is because of underlying infection going by the
leucocytosis
20:35 - : Can any of you share
the previous DKA protocol I had shared last time? Was unable to locate it again
this time
20:35 - : This message was deleted
21:14 - : The flowchart in this
is good sir
21:14 - : Her current GRBS is
122. Should I Give Dextrose and stop insulin sir ?
21:14 - : Give dextrose but don't
stop insulin. If necessary give 25% or 10% dextrose.
21:19 - VP: Sir, you asked to
continue insulin to prevent ketosis?
21:21 - RB: 👍
21:23 - RB: She's in ketosis.
This is to reduce ketosis by
correcting her insulin deficiency?
21:28 - RB: Currently giving 5D
according to the flowchart in the PDF I shared sir
21:28 - RB: Insulin currently
going in 0.5ml per hour.
21:29 - VP: How is her symptoms
now sir?
21:29 - VP: which PDF sir?
21:31 - The advantage here
is that the values are not in mmol but in mg per dl
21:31 - VP: pH was very low!!
21:31 - VP: She has UTI?
21:32 - : Not sure
21:33 - VP: There were 8-10 pus
cells
21:34 - : In women more than 10
would be suggestive but again uti is more likely
21:36 - : Subjectively how is she
feeling now?
21:36 - her dyspnoea
subsided
21:36 - : Vomiting?
21:36 - : no fresh episodes of
vomiting
21:53 - VP: Oh okay sir. Since,
her HbA1c was good. She may be getting recurrent episodes of infections eg, UTI.
21:53 - VP: This message was
deleted
21:53 - VP: Thanks sir
21:56 - : Not oriented to time
place or person sir.
21:56 - : GCS is 15 though.
21:56 - : yes sir we have advised for irine cultures
21:56 - : Sharing my notes on this patient. Request discussion and inputs on
it.
21:59 - VP: I liked this note
sir. They have mentioned clinical reasoning behind any decision
22:43 - : Aditya's Note
07:54 - : Sir her current GRBS
shot up to 362. Increased insulin to 3ml per hour
07:54 - : Re instituted 0.9 NaCl
@ 250ml per hour.
07:54 - : Yes as soon as you
added 25% dextrose you could have added more insulin per hour.
In DKA one never reduces the
insulin drip rate. Only dextrose needs to be adjusted
07:56 - : Urine output from 6pm
to 11pm was 1400ml
07:56 - : Input from 6pm 1900ml.
07:56 - : As she has no fever.
The IO chart is also covering insensible water losses indicating adequate
hydration.
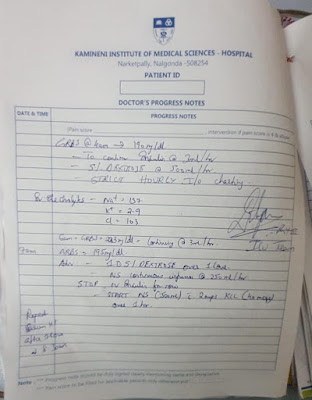
07:56 - : Hydration - Adequate
Bicarbonate - Not required
Insulin requirement - Matched to
target 200mg/dl
Potassium - will repeat serum
electrolytes
07:56 - : Urine output from 12 to
1 30 is 1000ml
07:56 - : Input also 1000ml
07:56 - : Current GRBS @ 299
07:56 - : Borderline K+
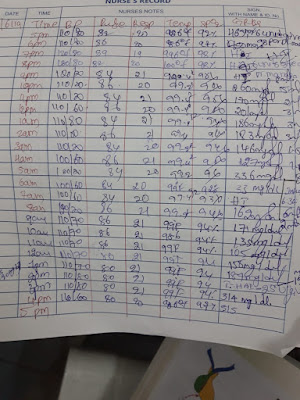
07:56 - : IMG-20190626-WA0000.jpg (file attached)
07:56 - : GRBS @ 200 at 3 am.
07:56 - : Electrolytes will be available shortly.
07:56 - : Current GRBS at 91.
Administering 25D with Insulin at 0.5ml per hour.
07:56 - : GRBS at 7 was at 73.
Stopped Insulin. Advised 25% Dextrose. Halfnor 1L in 1 hour.
07:56 - : Now at 249. Halfnor @
1L an hour advised.
07:56 - : Should we now switch to
S.C. insulin 2 hourly sir ?
07:56 - : Her urine for ketones
is still positive (sample sent at around 12 midnight)
08:11 - : By how much does the
10% dextrose increase the blood sugars level? And how much insulin is needed to
neutralize the dextrose we give?
08:11 - Are ketones
osmotically active like glucose?
08:11 - : Why is it that inspite
of giving IV Insulin, the patients potassium is still normal?
08:11 - : 45 female dki
Grbs at 11 am 130 mg/dl
Increased 10d
Currently dextrose rate 40 drops
per min
08:11 - : I.e 2.5 ml/min
08:11 - : Insulin 6u/hr
08:11 - : Dki patient grbs 159 at
12 pm
08:11 - : 👍add more dextrose? Recheck
ketones?
08:11 - : 25% drip rate can be
managed better without increasing fluid overload?
08:11 - : In a span of 1hr that
is from 11am to 12pm 10.5 gm of dextrose was delivered which increased body sugars
from 130 to 152 mg/dl which means 1gm of dextrose is increasing body sugars by
2mg/dl...hope this continues further..now we are continuing the drip rate at
0.2gm of dextrose per min which will deliver 12gm od dextrose over 1hr
08:11 - : 👍any reference links?
08:11 - : sir this is wat
happened in this 1hr in this pt
08:11 - I know but any
reference links to what has happened in the past 100 years to countless
patients?
08:11 - :
https://emj.bmj.com/content/22/7/512
08:11 - : ohk ..will luk for it
08:11 - : urine for kb sent at
11:30am is negative
08:13 - : Shall we switch to
subcutaneous then? What does your protocol say?
08:13 - : Sir but I remember when
we discussed the other day, the point bought out was Ketones will be taking
atleast 48-72hrs to become negative?
08:13 - : Based on what past data
from what studies?
08:13 - : When we were discussing
about patient the last time, when her urine for ketones were negative in 1
day, I remember someone raising this point sir.
08:13 - : Ketones will be
positive for atleast 48hrs.
But then have to review
literature on it
08:13 - : Yes let's find what's
mentioned in past literature based on previous observations by people like us
08:13 - : 1pm 196
2pm 182
3pm 171
08:13 - : So I'm stopping insulin
drip
And keeping her on hai s.c
08:13 - : Alright is she able to
eat?
08:13 - : If not then you may
switch her to algo 2
08:13 - : She is willing to eat
08:13 - : Grbs at 4pm 143
08:13 - : So 1.5 U per hour?
08:13 - : As long as she's out of
DKA do we need to worry about correcting insulin deficiency?
08:13 - : The algo you shared is
about treating high glucose and not DKA
In DKA we would need to maintain
the same amount of steady insulin flow and also infuse glucose to prevent
hypoglycemia
08:13 - : ya the algo which i
shared now is not for dka but i was thinking wat if her ketones were still
positive then we need to have increased it
08:13 - : Check again if they are
still positive.
Actually Rotheras is a bedside
test and children with type I are taught to play test it themselves
08:20 - : GRBS of Patient with
DKA 315 mg/ dl
08:20 - : 8pm and 10pm?
08:20 - : Her Urine for Ketones
are Positive again. Reverting to DKA Algorithm.
08:20 - : Did we continue iv insulin algorithm 1 or 2 or did we switch to subcutaneous before checking on the ketones again?
08:20 - : Is she 45 years old?
08:20 - : Yes sir.
08:20 - : Switched to
Subcutaneous Sliding scale sir. Sent for Urine Ketones and once it was positive
Switched to Algo 1 for DKA
08:20 - : after stopping dka
protocol ..thought of starting sc insulin from night but then she dint eat in
the night .. and her sugars went upto 350 so started on algo 2. and sent for
urine for kb which turned out to be positive then reverted to dka algo
08:20 - : Yep.
08:20 - : However with her K+
currently at 2.9. IV insulin is stopped and only Fluids with KCL therapy is
ongoing. This is according to the algorithm.
08:20 - : dextrose over 1hr???
08:20 - : No I stopped it because
Insulin had to be stopped.
08:20 - even while insulin
infusion ..is it recommended to give too rapidly?
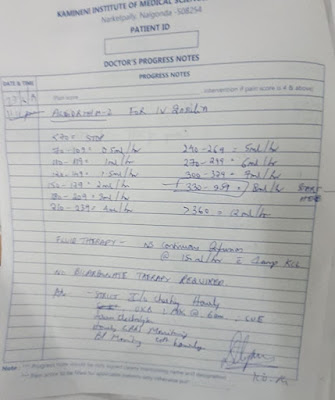
08:20 - : When Plasma Glucose
reaches 200 give 5D @ 250ml per hour. If less than 200. Rapid infusion may be
given.
08:20 - : Which algorithm
advocates stopping insulin in DKA?
Please quote with link
08:20 - : Also 5D is not a good
resuscitation fluid. So fluid overload unlikely.
08:20 - : The statement appears
contradictory
08:20 - : Sir this picture taken
from the PDF I shared says Hold insulin if Serum K+ less than 3.3
08:22 - : Hold Insulin? What
evidence do they have for making that statement?
Can't agree unless there is more
evidence for that decision.
It's not hypokalemia that kills
but dka can
08:22 - : Also 40MeQ over one
hour as per your notes is too fast for what the protocol advises?
08:22 - : Sir it's in the picture
I shared. And when I looked for a reference they cited their own article.
(Reference 13)
08:22 - : The picture says 20-30
MEq per hour
08:22 - : Yes sir. We are giving
it over 90 mins sir. I changed it after taking the pic sir.
08:22 - : Add it in the file as a
separate note and share the picture of your note again but don't change your
initial note
08:22 - : Unfortunately I already
did it sir. I will write it again sir
08:22 - : And remember whatever we write in
our progress notes is our plan.
What we write in the nurses order sheet is
what is legally executable.
Ideally the nurse is not supposed to execute
what you write in the progress notes
08:22 - : Sir her current GRBS is 194.
08:22 - : 6 shy of the minimum mark.
08:22 - : Numbers are at best an
approximation.
There are no real validated cut offs.
What experiments have these guidelines been
based upon? Were we able to review those?
08:22 - : You can also use 10% or even 25%
dextrose as the glucose drip rate can be titrated lower to prevent fluid
overload and if you can share it as a thesis in 100 patients they will invite
you to rewrite the guidelines
08:22 - : Okay sir. Will start with 10D over
2 hours ?
08:22 - : Either way you will need to watch
her for hypoglycemia with hourly checking of sugars to anticipate how much you
need to increase the dextrose drip rate to prevent hypoglycemia.
Does your dextrose serve any other purpose
right now other than preventing hypoglycemia in this patient?
08:26 - : Is she 45 years old?
08:26 - : Yes sir.
08:26 - : But the BMJ Case reporters have
been thinking her to be 55 years old 🤔
https://docs.google.com/document/d/1RYmcszyce2l02vvmj2tst4cdS79bTfxnAsmOmkfohpM/mobilebasic
08:29 - : "A 55 year old female,
agricultural labourer by profession"
Wish I could know more about her as a person.
How does one become an agricultural laborer in Telangana? What was her career
path that she followed?
09:00 - MS: The son in law told as an
estimate that she would be around 55 years sir.
09:01 - MS: Polam and kuli panulu cheskuntam
sir (words of patient) - agricultural and daily wage labourer sir
09:12 - : Yes that's what the English also
says.
I wanted to know her details as a person.
How does one become an agricultural laborer
in Telangana? How did she become one?
Knowing her story in detail would enable me
to connect better with her not only in this crucial critical point in her life
but also hopefully later
20:35: Grbs of dki 506mg/dl
20:35: Was the insulin 6U per hour held for a longer
duration?
Please tell us since when is she currently on the 6U per
hour and for how long it was stopped.
Also ensure that we never stop it till the ketones are
negative.
Just stop the dextrose and titrate it again at 150 and the
same holds for the potassium
20:35: She was maintained on 3U/hr as her GRBS was
maintaining between 200 to 300 sir. However when Serum K+ was detected to be
low, that was when we had to stop insulin according to the protocol and start
KCL therapy sir. At 8 her GRBS was 194 and we advised for 10D.
20:36: How long was it stopped?
20:36: for around 3hrs
20:36: and she had idli in the morning
20:36: morning urine for kb is positive
20:36: So,again iam starting insulin 6units per hr
20:36: for potassium replacement ..40meq given and sample
sent ..report awaiting..should we start k+ too along with insulin or wait for
k+report and then start k+ infusion??
20:36: sir the acidosis is due to ketones is it ..but here
the acidosis has improved but still the urine ketones are positive
20:36: 40MeQ only given? How much contribution does it make
for her total body potassium? Use the formula?
20:36: She's still acidotic. Just CO2 is compensating
20:36: ohk
20:36: sir you said we need to target the ketonuria ..but
then acidosis would be better as it would reflect the plasma ketones
20:36: and plasma ketones are more reliable than urine
ketones
20:36: acc to the formula ..at k +of 2.9 she has a deficit
of 85meq
20:36: Then why did we stop at 40?
20:36: That would be a nice thesis
20:36: the level of k+ rise is different im different
articles sir..but in the book its given 20meq will raise serum k+ by 0.25meq
20:36: Grbs of dki patient 510mg/dl
6u /hr I.v infusion and ns infusion is going
20:36: increase insulin
20:36: How much increase would you do if this was algo 2 or
1?
20:36: 12u
20:36: In algo 1 or 2?
20:36: algo 2
20:36: Let's go slow with it and use algo 1 to escalate.
So the learning is if we need to increase insulin in DKA we
use algo 1 or else we continue DKA algorithm
20:48: dka pt : grbs 283mg/dl @5:00pm
insulin
drip @4ml/hr
20:48: How many units per hour?
20:48: 4units
20:48: Are we supposed to come down below 6U in DKA ?🤔
20:48: yes sir ..we can but not below 0.05U/kg/hr
20:48: We can? How?
Don't tell me because it's given in the cookbook but let me
know the logic or experimental evidence for it if available
20:48: sir u said ketosis is a reflection of insulin defeciency
but why not bs can also be a predictor of it??
20:48: Now dki Grbs 310
7units/hr I.v insulin is going according to algorithm 2
Sr.pottasium sent at 5pm __ 3.4
Urine for ketone bodies negative
20:48: Continue algo 2 👍
20:48: sir we shall continue the dka protocol till 8:30pm
then again repeat urine kb and abg if kb is neg and hco 3is more than 17 and if
the pt is eating then will overlap with sc if she is not eating then algo 2??
20:48: Yes both of these are dependent on insulin deficiency
but while ketones can be made zero blood sugar can't
20:48: Good plan 👍
20:49: ya ..sensible!
20:49: sir only difference i notice in algo 2 and dka
protocol is we are supplementing with dextrose with low BS ..
20:49: in case of dka
20:49: Also we are increasing insulin dose in case of higher
sugars
20:49: with higher sugars we are anyway following algo 2 no
sir even in dka
20:49: The correct English would be:
"It makes sense"
Pardon my English teaching addition to the conversation
20:49: Yes but that is not mentioned in any DKA protocol?
We just made a modification of it ourselves and will
hitherto become a short note as "XYZ DKA protocol."
20:49: sir its given we can titrate it but not less than
0.05u/kg/hr
20:49: sr k+from 11am to 5pm (6hrs)has dropped to 0.5meq
with 34U of insulin
20:49: Good documentation. Any literature on similar rate of
fall with Insulin documented elsewhere?
20:49: sir the present k+is 3.4 ..so shall we supplement
with 1amp ..hope it would increase the sr k+ by 0.5 in this pt coz previously
with 40meq it increased k+ by 1meq
20:49: we can decide to maintain the target k + around 4
08:17: 45F with DKA . Urine for Ketones positive again.
08:17: Initiating DKA Algorithm 1
08:17: ph 7.5?
08:17: Current GRBS 347. Insulin infusion @ 7units per hour.
Potassium 20meqs in 1 pint NS
08:17: She doesn't require bicarbonate
08:17: Yes. Apologies for the poor handwriting.
08:17: titrate insulin acc to algo 2but not less than 3ml/hr,if
grbs around 170 then supplement with 10%D at 40drops per min
08:17: Okay.
08:17: 216 at 4am and just checked now her GRBS is at 49. Going by
algo 2, stopped insulin and gave 25D.
08:18: 45F with DKA
S - Patient feeling well. She has no fever and able to eat
O - Hemodynamically stable with one episode of Hypoglycemia at
5am. Corrected with 25D and eventually improved to 219 at 7am. Serum K+ at 2.8.
Other lab parameters within normal limits. I/O 4400/4350 at 7 am.
A - Morning urine for ketones awaited to tweak plan. ABG normal.
Fluid management adequate.
P - At least 2 consecutive samples of urine should be negative for
ketones. Fluid management with Dextrose supplementation and KCl supplementation
as required. Encourage oral feeds.
08:18: Ketone Bodies Negative. To continue Algo 2 ?
08:18: holding the insulin for a while during k+supplementation
logically makes sense coz may be if we continue insulin that would push k+ into the cells
08:18: No it doesn't because we are trying to treat insulin
deficiency and not potassium deficiency caused by exogenous insulin. The
logical solution for potassium deficiency caused by exogenous insulin while
treating insulin deficiency would be potassium supplementation?
Question is how much potassium would one need to supplement during
iv insulin administration to prevent extracellular potassium deficiency?
08:18: sir should we continue dka protocol and send another sample
of urine or start with algo2??
08:18: We are already giving her a hybrid protocol combining both
but let's hit the ketones (insulin deficiency) hard .
Continue DKA algorithm till three consecutive ketones are
negative.
Check her hospital bills. Is she paying for all that we are doing?
08:18: yes sir she is bearing all the charges
08:18: Let's ask for academic free. Don't you feel guilty about
learning so much from her for free? 🤔
08:18: and only her daughter accompanies her everytime
08:18: What's her source of income? 🤔
08:18: Above was yesterday's conversation
08:18: Below is today's
08:20: Her daughter and da daughters husband are into
agriculture.. so they get money every 6 months.. Right now they borrowed money
from someone else to pay their hospital bills.
08:20: She has son also but he ran away from the house.. And the
patients husband is also doing agriculture
08:20: Yes her son ran away before her first admission which may
have precipitated her first attack of DKA.
45F with DKA. 3 consecutive urine samples are now negative for ketones.
08:21: 45F with DKA
S - Patient feels well. Frustrated with too pricks and injections.
Ate well yesterday. Wants to eat well now.
O - Hemodynamically stable. 3 consecutive samples of urine
negative for ketones. 1 episode of Hypoglycemia (GRBS 39 at 4am - Improved to
146 by increasing 10D flow). She is currently on subcutaneous insulin 2 hourly.
I/O 5300 / 5000 ml.
A - Mild hypokalemia (3.3) neither improving nor worsening with
40meqs every 4 hours. Occasional episodes of hypoglycemia not followed by
morning hyperglycemia. Able to eat well.
P - She needs adequate hydration and glycemic control. Can
deescalate to 7 point profile and HAI with Mixtard today? Needs to be properly
counseled about DKA and its precipitating factors.
08:21: Is she really 45 years old? Please recheck with her
relatives
08:21: Yes sir. Just confirmed.
08:21: 👍Good note
What would you counsel about her precipitating factors? What do
you think is precipitating her DKA everytime she's gotten admitted?
08:21: Could suspect a UTI in a diabetic woman sir.
08:21: What's her urine culture showing? We had even visited
Microbiology yesterday to look at it but I forget if we were able to trace it
08:21: What was the cause in her previous admission?
08:21: Her urine for ketones this morning is negative. 4
consecutive samples.
08:21: Her electrolytes are exactly the same.
08:21: Good. Let's put her on a physiological subcutaneous insulin
regime as you suggested above
08:34: sc insulin every 2nd hrly??
08:34: No.
Before meals short acting and subcutaneous nph twelve hourly
08:34: The nph can be mixed with the short acting before breakfast
and dinner
08:34: She again had one episode of hypoglycemia GRBS 58. Now @
182
08:34: ohk sir...will calculate the requirement and accordingly
advise
08:34: When is she going to have her breakfast?
09:14: sir the total dose from yesterday is coming around 128
units...and if we divide it into bd dose it’s cuming to morning 56 u and nite
30units
09:14: Bd Dose is not physiological.
She needs the short acting before every meal and the long acting
only twice.
The short acting can be mixed to the long acting twice before
breakfast and dinner. The lunch would need a short acting before.
We can begin with
Short acting 6U +Long acting (mixtard) 6U before breakfast, before
lunch short acting depending on pre lunch, before dinner short same dose as pre
breakfast but again titrated to pre meal sugar values
20:24: She ate 2 chapathi's at 2 pm and 25units of hai was given
20:24: Now her sugar are 111mg/dl
We didn't give insulin to her
20:24: Grbs at 6.pm 43mg/dl
Advising 25 d
20:24: put it slowly..coz again it will be difficult to know the requirement
20:24: Only half 25d was given now at 7pm sugars 341
20:24: She's very prone to hypoglycemia and it's getting difficult to predict and optimize her insulin.
I guess we will need to come down in our insulin dose and ascend in small increments. So although my plan of 6U day before yesterday was too conservative and she ended with "hi" we shall need to strike middle ground. If you look at our breakfast plan of mixtard 30 and actrapid 10 made today at 12:22 PM if you scroll the messages above, you will find that it amounts to just 19U of actrapid.
Inspite of that we calculated 25U before lunch.
Also what is her renal function? Can she tolerate long acting insulin?
20:25: When is she taking her dinner?
20:25: sir we started sc from lunch ,she hasn’t received morning dose,
20:25: Her Sr. Cr. 0.51 sir. She can for that eGFR sir.
20:25: It is 138 sir her eGFR
20:25: She will have her dinner shortly sir
20:25: Yes
20:25: What dose should we advise pre dinner sir ?
20:25: Instead of the afternoon planned 30+10 for her dinner let's come down to 20U of Mixtard (containing 6U of actrapid) and mix with 6U of actrapid.
Going by her afternoon response to actrapid it appears that the actrapid was behaving like a long acting with no obvious peak effect in two hours of her lunch but the insulin effect only peaked four hours later.
So be careful about what happens to her tonight four hours later.
Not sure why her actrapid insulin kinetics has changed. Is it a problem with the company? What brand is she getting? Or is it a problem with her body's response?
20:25: Current GRBS 114
20:25: Wait a minute.
From 7 PM with her sugar of 341 how did it come down to 114 now?
Is this after her pre dinner insulin already taken?
20:25: It was given right before her dinner sir. And this value is right after dinner sir.
20:25: 114 right after?
20:25: Dinner was somewhere around 9:00 PM?
20:25: Started at 9 05 and ended at around 9 20 sir
20:25: OMG. It appears that her previous insulin was still actively bringing her sugars down.
Somehow that short acting actrapid 25U before lunch is having a longer effect of hypoglycemia.
Please watch out hourly. Does have hypoglycemia unawareness too? Are we able to see symptoms when we find her to be 40-50 or are these incidental detections?
20:25: No sir. She never reported symptoms of hypoglycemia during my watch.
20:25: Even during my duty I was consistently asking about hypoglycaemic symptoms but she didn't tell any
20:25: 126 now sir
20:25: Current GRBS 120
20:25: Current GRBS 98
20:25: 10D on Standby.
20:25: Current GRBS @ 45. Advising 10D slowly to keep it non aggressive.
20:25: Still @ 47. Increasing 10D before I move over to 25D.
20:25: Now @ 122
20:25: Did not need 25D.
20:25: Current GRBS @ 87. Slightly increased 10D to maintain it there.
20:25: Now @ 197. Maintenance with 10D ongoing.
20:25: Now @ 89mg/dl. 10D is being titrated accordingly.
20:25: GRBS now @ 312. Stopped 10D completely.
20:26: Looks like we shall need to avoid any long acting insulin in her completely as even the short acting insulin is behaving like long acting in her system although her eGFR appears normal (btw what was the date of that creatinine test?)
8:54: Sir nw grbs is 231
How much insulin to be given sir ?
Ystdy (1/07/2019) after giving 6u in mrng sir
8:55: Yes but yesterday she was also under the influence of day before yesterday's mixtard and day before yesterday she had had hypoglycemia at night early morning which seems to have worn off yesterday night early morning.
I was thinking we can give her 8U before breakfast today but let's give her 6U before breakfast now
02/07/2019
8:33: Looks like her 12U before lunch was going strong acting for long to dip her morning sugars. I guess she remains unaware of her hypoglycemia every time we record it?

















Comments
Post a Comment